Living with a chronic or complex condition often means long-term treatment—and that can come with high costs and limited options. Biosimilars are changing that. These medications are designed to work just like existing biologic drugs but are typically more affordable, offering another safe and effective way to manage serious health concerns.
As more biosimilars become available, they’re offering hope to people who need ongoing care. Whether it’s for autoimmune conditions, cancer, or other long-term illnesses, biosimilars make it easier to access treatment while reducing financial stress.
Here’s what you need to know about them.
Introduction to Biosimilars
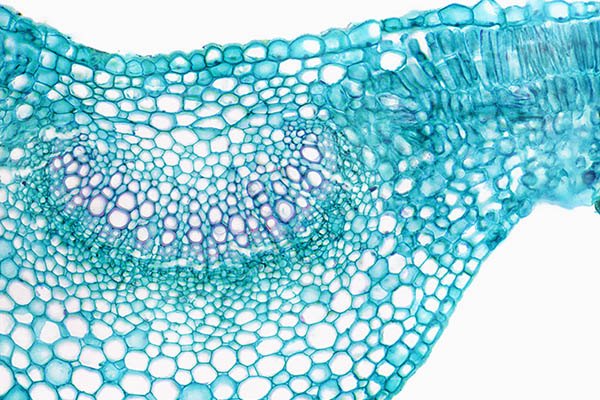
If you’re managing a long-term condition, you’ve probably heard about biologic medications—powerful therapies made from living cells that are used to treat complex conditions like autoimmune diseases, certain cancers, and more. Unlike traditional drugs made from chemicals, biologics are produced using living organisms, which makes them more complex and often more expensive.
Biosimilars are a newer option that work in almost the same way, but they’re made by different manufacturers and often come at a lower cost. That makes it easier for more people to access the treatment they need without sacrificing safety or effectiveness.
Across the healthcare world, biosimilars are helping expand treatment choices and reduce costs—while still maintaining high standards. For patients, that means having more options, more support, and more peace of mind.
What Exactly is a Biosimilar?
A biosimilar is a medication that’s been approved by the Food and Drug Administration because it’s been shown to be highly similar to an existing biologic drug—what’s called a “reference product.” It delivers the same treatment benefits and meets the same safety and quality standards.
Biologics are made from living cells, so there’s always a bit of natural variation. Biosimilar medications are developed within very tight boundaries to make sure they work just as well, even though they’re not identical down to every molecule. They go through rigorous testing to ensure they provide the same results—and that gives both providers and patients confidence in their use.
Many biologic medications—and their biosimilar counterparts—are large, complex molecules that can’t be taken orally because they’d break down in the digestive system. Instead, they’re given by infusion (IV) or injection, depending on the drug and condition.
So if a patient is prescribed a biosimilar version of a biologic drug that requires IV delivery (like infliximab or rituximab), they’ll receive it through infusion therapy in a clinic, hospital, or infusion center.
Biosimilars versus Biologics
Biologics and biosimilars are both advanced medications made from living cells, often used to treat serious or long-term conditions like autoimmune diseases or certain cancers. While they work in similar ways, there are a few key differences that are helpful to understand:
- Biologics are the original medications. They’re developed through a lengthy research and approval process and are often protected by patents when first released.
- Biosimilars are newer versions made by different manufacturers after the original biologic’s patent expires. They’re designed to be highly similar in how they work, how they’re given, and how safe and effective they are.
Whether your provider recommends a biologic or a biosimilar, you can feel confident that both options are safe, effective, and held to strict quality standards. Biosimilars simply offer another path to proven treatment—often with fewer barriers to care.
How Biosimilars Are Developed
Biosimilars go through a thoughtful, highly detailed development process to make sure they’re just as safe and effective as the original biologic drugs they’re based on. Every step is guided by science, from selecting the right cell lines to carefully studying how the medication performs.
Before a biosimilar ever reaches a patient, researchers run tests to confirm that it closely matches the original medication in structure, function, and results. It’s a rigorous journey—but it’s worth it. The result is a treatment that offers the same benefits, giving patients more options without compromising on quality of care.
Manufacturing and Quality Control
Because biosimilars are made from living cells, their production takes place under tightly controlled conditions. Scientists monitor everything—from temperature to pH levels—to make sure each batch is consistent and reliable.
Even small changes in the manufacturing process can affect the final product, so quality checks happen at every stage. These checks confirm the biosimilar’s strength, purity, and overall makeup. That way, patients and providers can feel confident knowing the treatment meets the highest standards—every time.
Regulation and Approval
Before a biosimilar can be used in the real world, it has to prove itself through a thorough approval process. That includes lab testing, clinical trials, and side-by-side comparisons with the original biologic drug.
Regulatory experts review the evidence closely to make sure the biosimilar works just as well and has a similar safety profile. Once approved, the medication continues to be monitored to ensure it performs the way it should. This kind of oversight helps patients feel supported and reassured—knowing their treatment is both trusted and tested.
How Biosimilars Are Used in Treatment
Biosimilars are becoming a trusted part of care for people managing chronic and complex conditions—especially in areas like cancer treatment and autoimmune diseases. These medications offer the same therapeutic benefits as the original biologic drugs but often at a lower cost, making long-term treatment more manageable.
When considering a biosimilar, healthcare providers take a close look at each patient’s health history and current treatment plan. If a biosimilar is a good fit, it can offer relief without adding financial strain. For many patients, that means staying on track with essential therapy and feeling confident in the care they’re receiving.
What Health Conditions Do Biosimilars Help Treat?
Biosimilars are used to manage several serious or long-term health conditions. They offer the same benefits as original biologic drugs but are often more affordable—making ongoing treatment more accessible for many people.
Here are some common conditions where biosimilars are used:
- Rheumatoid arthritis and other autoimmune diseases
Medications like Humira (adalimumab) can help reduce joint pain, swelling, and inflammation.- Examples of biosimilars: Simlandi (adalimumab-ryvk), Yuflyma (adalimumab-aaty), and Idacio (adalimumab-aacf)
- Certain cancers
Biosimilars of drugs like Herceptin (trastuzumab) are used in cancer care to target specific tumor cells.- Examples of biosimilars: Ogivri (trastuzumab-dkst), Herzuma (trastuzumab-pkrb), and Ontruzant (trastuzumab-dttb)
- Crohn’s disease and ulcerative colitis
Medications such as Remicade (infliximab) can ease digestive inflammation and symptoms.- Examples of biosimilars: Inflectra (infliximab-dyyb), Renflexis (infliximab-abda), and Avsola (infliximab-axxq)
- Plaque psoriasis and psoriatic arthritis
Treatments like Stelara (ustekinumab) can help manage skin and joint symptoms in chronic inflammatory conditions.- Examples of biosimilars: Wezlana (ustekinumab-auub), Selarsdi (ustekinumab-aekn), and Pyzchiva (ustekinumab-ttwe)
These biosimilars are carefully tested to ensure they work just like the original biologics. That means patients can feel confident they’re getting safe, effective treatment—without the high costs that often come with long-term care.
Are Biosimilars Safe and Effective?
One of the most reassuring things about biosimilars is that they work just as well as the original biologic drugs. They have been shown to provide the same level of symptom relief, have similar side effect profiles, and deliver consistent results over time.
Before any biosimilar is approved, it goes through a rigorous evaluation process to confirm its safety and performance. And even after it reaches the market, ongoing monitoring continues to ensure the medication remains a safe and effective option.
Most patients and providers find the transition to a biosimilar to be smooth—and the added benefit of lower cost makes these therapies an increasingly popular choice for long-term care.
How Biosimilars Can Make Treatment More Affordable
Biologic medications can be life-changing, but they’re also expensive. For many people, the high cost of treatment can be stressful and even limit access to care. That’s where biosimilar medicines come in.
These medications offer the same safety and effectiveness as the original biologics but usually at a lower price. As more biosimilars become available, competition increases, which can help bring down prices even more.
This kind of shift doesn’t just help healthcare providers—it helps patients, too. Lower costs often mean more people can start or continue important treatments without worrying as much about the financial impact.
Real Savings for Patients and Healthcare Systems
Biosimilars are designed to help ease the burden of long-term care—not just for individuals, but for the healthcare system as a whole.
Here’s how they make a clinically meaningful difference:
- Lower costs for patients: People who need repeated or ongoing treatments may pay less out of pocket.
- Fewer barriers to care: Lower prices can make it easier to stick with treatment plans over time.
- Smarter use of healthcare dollars: Clinics and hospitals can invest more in patient care, education, and technology.
- More room in insurance budgets: Insurance companies may pass savings on to patients through better coverage options.
These savings create more flexibility—so patients get the care they need, when they need it.
Insurance and Coverage
Insurance plans are starting to take a closer look at biosimilars—and many now list them as preferred treatment options. This change is based on strong clinical evidence and the potential for significant cost savings.
If you’re considering a biosimilar, it’s a good idea to check in with your provider or care team to confirm your coverage details. Some treatments might require prior approval, but your provider can help you navigate the process.
Having that conversation upfront can prevent delays and make sure your therapy stays on track—without putting extra strain on your budget.
Biosimilars vs. Generic Drugs
It’s normal to get confused when comparing biosimilars to generic drugs, but they’re not quite the same thing. While both are designed to offer more affordable alternatives to brand-name medications, the way they’re made and tested is different.
Generics are exact copies of the original drug, made with the same chemical formula. On the other hand, biosimilars are based on complex therapies that are grown from living cells. They’re not identical to the original biologic treatment, but they’re carefully tested to make sure they work in the same way and provide the same benefits.
Key Differences
Here’s where the two differ:
- Generics: These are made to be chemically identical to the brand-name drug. If the original medication has a precise molecular formula, the generic version matches it exactly.
- Biosimilars: These are modeled after biological medicines—large, complex molecules produced from living cells. Because of the way they’re made, biosimilars can’t be an exact match. Instead, they undergo thorough testing to ensure they work in the same way as the original biologic.
Creating biosimilars takes more time and effort than making a chemical-based generic because of their complexity. Scientists conduct detailed side-by-side comparisons to make sure the biosimilar has the same safety, stability, and effectiveness as the original biologic.
What This Means for Patients
Choosing a biosimilar can mean significant savings for patients, as these therapies typically come at a lower price than their reference biologics.
Providers will monitor your progress to make sure the biosimilar works as expected, checking for any changes in how you’re managing symptoms. If all goes well, you might enjoy long-term savings without losing out on effectiveness.
It can also be reassuring to know that biosimilars go through strict approval processes before they can be prescribed. Insurance companies often expand their coverage once they see the data supporting these therapies, making it easier for you to stay on treatment without worrying about costs. This can take a lot of the stress out of managing your care and help you feel confident that you’re getting the best treatment for your needs.
Biosimilars and the Future of Accessible, Effective Care
Biosimilars are making a real difference for people facing ongoing health challenges. By offering a more affordable option while delivering similar benefits to established biologics, they’re gaining attention from healthcare providers, insurance providers, and patients.
More and more people are finding that switching to a biosimilar can provide the same results with fewer financial concerns.
If you’re considering a biosimilar or changing therapies, it’s important to discuss it with your healthcare team to ensure it’s working for you.
At CSP, we’re here to support you. If you have questions about biosimilars or your treatment options, reach out to our team. We’re committed to helping you find the best care for your health journey.
Frequently Asked Questions (FAQ)
What is a biosimilar with an example?
A biosimilar is a biologic medication that’s highly similar to an already approved biologic, also called the reference product. For example, Zarxio (Filgrastim-sndz) is a biosimilar of Neupogen (filgrastim).
What is the difference between biosimilar and generic drugs?
Biosimilars are biologic medicines made from living organisms, and while they’re similar to their reference products, they’re not identical. Generics, on the other hand, are exact chemical copies of brand-name drugs.
What is the purpose of biosimilars?
Biosimilars offer a more affordable and accessible treatment option for patients by providing alternatives to existing biologic medicines. They help reduce healthcare costs while maintaining effectiveness.
What is the difference between a biosimilar and a biologic?
A biosimilar is designed to be highly similar to an existing biologic, but it’s made by a different company. While they’re very close, biosimilars might have small differences in certain components that don’t affect how the medicine works.
The content provided on this blog is for informational purposes only and does not constitute medical advice, professional advice, or a recommendation regarding any particular course of treatment. While we strive to provide accurate and up-to-date information about the role of specialty pharmacies in the adoption of biosimilars, the information shared here is based on publicly available sources and is not intended to replace professional medical consultation or advice.
The use of biosimilars and other medications should always be discussed with a healthcare provider who can evaluate the appropriateness of any therapy based on individual circumstances.
By accessing this blog, you agree to hold harmless the author, publisher, and any associated parties from any claims, liabilities, or damages arising from the use or interpretation of this content.
©2025 California Specialty Pharmacy, LLC. All rights reserved.